If you are frustrated with psoriasis flares, identifying causes can be difficult because:
- Immune responses are unique.
- Trigger-to-flare delays extend 2 weeks or more.
Some common culprits may be triggering your flares.
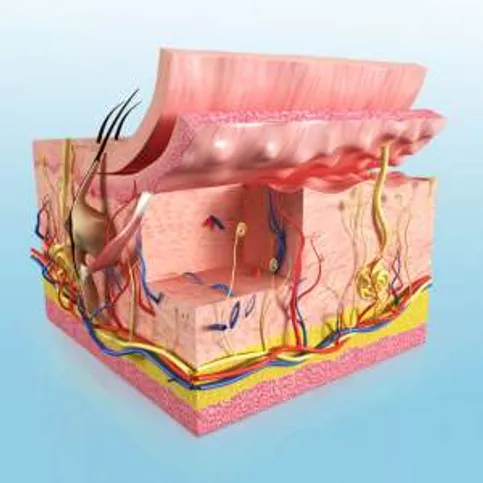
Skin Injuries
Bug bites, needle pricks, cuts or burns can trigger a Koebner response. Plaque lesions mimic the original injury on healed skin. Early medical intervention can treat the reaction, but you can prevent injuries by avoiding risky behaviors such as tattoos and using:
- Sunscreen.
- Insect repellant.
- Protection for high-impact activities.
- Care with razors, knives and dangerous objects.
Ordinary Infections
Flares may follow minor illnesses:
- Cold viruses.
- Earaches.
- Bronchitis.
- Tonsillitis.
- Flu.
- Staph.
- Fungal infections.
- Strep throat.
Treat infections early to prevent flares. Even if you are asymptomatic, doctors recommend testing for strep throat.
Alcohol
Just two drinks a week may cause a flare. Alcohol:
- Renders psoriasis medications ineffective.
- Dehydrates already dry, flaky skin.
- Contributes to weight problems and depression, which worsen psoriasis.
Smoking
Quitting may be stressful, but smoking increases the risk and severity of psoriasis flares. Delivering up to 7,000 chemicals, it also:
- Increases susceptibility to infections.
- Inflames the circulatory system — your skin’s source of healing.
Experts recommend using smoking cessation aids and support groups.
Temperature Extremes
Cold, dry climates aggravate psoriasis. So do extreme temperature changes in your daily routines:
- Taking hot showers or baths.
- Hand washing dishes, especially pots and pans.
- Handling frozen food or clearing icy windshields.
Instead:
- Choose moderate water temperatures.
- Use moisturizers and humidifiers.
- Keep gloves handy.
Sugar
Severe psoriasis doubles your likelihood of developing diabetes, which worsens flares. Controlling weight and blood glucose levels helps because fat cells in psoriasis patients secrete inflammatory hormones that increase insulin resistance. Try:
- Choosing fruit over refined sugars.
- Drinking beverages for thirst, not sweetness.
- Reading labels to avoid high-fructose corn syrup and reduce sugars (ingredients ending in “-ose”).
Gluten
Celiac disease may increase psoriasis risk. For some, wheat, rye and barley cause flares. Going gluten-free may be worth a try. Many gluten-containing foods are obvious. However, read labels on:
- Soy sauce.
- Chocolate.
- Alcohol.
- Deli meats.
- Soups.
- Salad dressings.
Medication
Many psoriasis patients have additional medical conditions, but prescriptions to treat them can exacerbate flares. Consider asking your doctor about alternatives to:
- Beta blockers containing propranolol (Inderal, Inderal LA, Inderide, Innopran XL, Propranolol Hydrochloride Intensol).
- Indomethacin-based nonsteroidal anti-inflammatories (Indocin).
- Lithium antidepressants (Eskalith, Eskalith CR, Lithobid).
- Antimalarials for lupus and arthritis — Atabrine (quinacrine), Aralen Phosphate (chloroquine) and Plaquenil (hydroxychloroquine).
- Quinidine heart medication (Quinidex).
- Interferon alfacon-1 for hepatitis C (Infergen).
Stress
The best thing you can do — the hardest, too —is to reduce stress:
- Systematically eliminate triggers.
- Track triggers and flares.
- Join support groups.
- Exercise.
- Try meditation or relaxing yoga.
- Always remember that you are not alone in the battle against psoriasis.